navigate By section
Mental Health
What is mental health?
Mental health includes our emotions, mind, and relationships with others. It’s displayed in how WE THINK, FEEL, AND ACT. It helps us determine how we handle stress, relate to others, and make choices. Mental health is important in every stage of life; from child, to teen, all the way through becoming an adult [1]. Mental health problems are common, but not everyone is diagnosed with a mental illness [2].
Your experiences with mental health challenges can be uniquely your own. Some have trouble doing things they like or need to do because of how they feel–like going to school, work or hanging out with friends; some may be feeling down or upset for long periods of time [3].
Remember that everyone goes through tough times, and no matter how long it’s been occupying your mind, it’s important to talk to someone about it like your parents/guardian, counselors, or family doctor. If you are experiencing suicidal thoughts or emotional distress help is available. Call the national suicide prevention lifeline at 988.
In Illinois, minors aged 12 and older can receive confidential mental health services, including counseling and psychotherapy, without parental consent. They also have the right to access and authorize the release of their own mental health records, and parents’ access is limited.
[1] Mental Health. (2020). What is mental Health. Retrieved from https://www.mentalhealth.gov/basics/what-is-mental-health [2] Centers for Disease Control and Prevention. (2018). Learn About Mental Health. Retrieved from https://www.cdc.gov/mentalhealth/learn/index.htm [3] Mental Health. (2020). Talk About Mental Health. Retrieved from https://www.mentalhealth.gov/talk [4] National Institution of Mental Health. (2020). Help for Mental Health. Retrieved from https://www.nimh.nih.gov/health/find-help/index.shtml
Positive Psychology
Positive psychology is the scientific study of what makes life most worth living [1]. Simply put, positive psychology is the study of happiness. This relatively new branch of psychology studies human thoughts, feelings, and behavior, with a focus on strengths instead of weaknesses, and building the good in life instead of repairing the bad [1].
When you think of traditional therapy, you might imagine a session where a psychologist asks personal questions to diagnose and fix problems with you and your family. Positive psychology flips this idea on its head. It doesn’t focus on what needs to be fixed, but rather on your strengths and what’s going well in your life. The great thing is, you can even practice many positive psychology exercises at home, either by yourself or with an adult.
Remember that everyone goes through tough times, and no matter how long it’s been occupying your mind, it’s important to talk to someone about it like your parents/guardian, counselors, or family doctor. If you are experiencing suicidal thoughts or emotional distress help is available. Call the national suicide prevention lifeline at 988.
Some Positive Psychology Exercises
The Three Good Things Exercise
Gratitude Journaling
Identify and Use Your Signature Strengths
Acts of Kindness
[1] Peterson, C. (2008, May 16). What Is Positive Psychology, and What Is It Not? Retrieved June 26, 2025, from https://www.psychologytoday.com/us/blog/the-good-life/200805/what-is-positive-psychology-and-what-is-it-not
Overall Wellness
When we think of wellness, we often only consider exercise and nutrition. However, wellness is much broader, encompassing our entire state of well-being, including many other aspects of our health beyond just diet and physical activity.
Physical
Nourishing a healthy body through exercise, nutrition, sleep, etc.
Mental
Engaging the world through learning, problem-solving, creativity, etc.
Emotional
Being aware of, accepting and expressing our feelings, and understanding the feelings of others.
Spiritual
Searching for meaning and higher purpose in human existence.
Social
Connecting and engaging with others and our communities in meaningful ways.
Environmental
Fostering positive interrelationships between planetary health and human actions, choices and wellbeing.
Your well-being is like a network of connected parts. It’s important to pay attention to your overall state of wellness because all these dimensions of health affect one another, which directly shapes how you feel, think, and act.
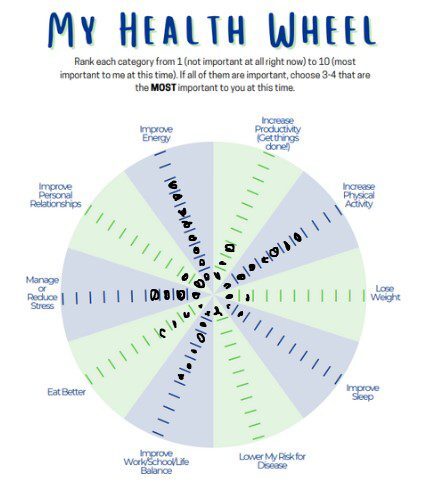
Find out where your state of wellness is by creating your own wellness wheel.
The Wellness Wheel Model represents our overall state of well-being. Within this wheel, there are separate slices and each slice represents a different dimension of health.
Try to identify your overall state of well-being by rating each dimension of health. To do this, shade in each slice to the appropriate line that best matches how important focusing on this dimension is to you and how it can help improve your overall wellness.
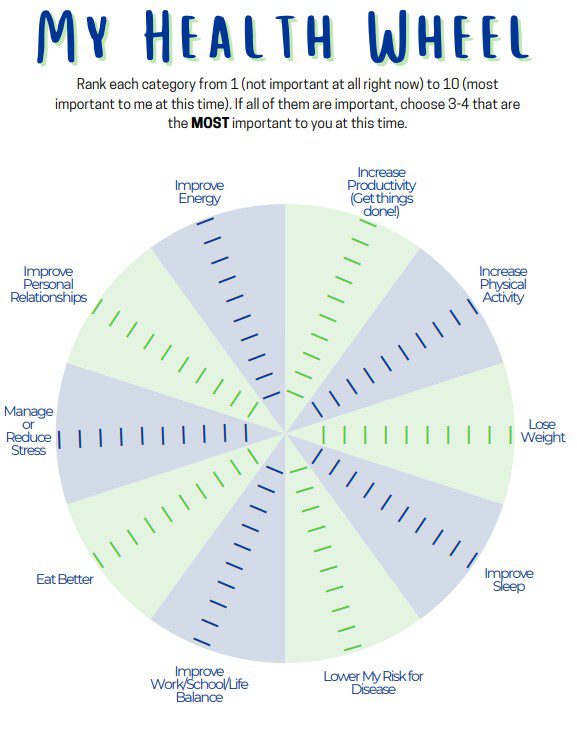
For example:
Someone’s wheel that looks like this would say that working to improve their energy levels (8) and the amount they are physically active (7) would be most important to them. Working to improve personal relationships (2), lose weight (2), improve sleep (2), and lowering risk for disease (1) are not important at this time.
This activity is a chance to pause and see where you might need support from a trusted adult to improve certain areas of your health. You might find you need a lot of help in some areas—or even all of them—and that’s completely normal. Others might need less help, and that’s okay, too. Remember, wellness is a continuous journey for everyone. There will be times in your life when you need extra support, and it’s always okay to ask for it.
[2] What is Wellness? (2019, May 14). Retrieved June 26, 2025, from https://globalwellnessinstitute.org/what-is-wellness/
Common Diagnoses
Occasional feelings of fear or worry are a normal part of life. If these feelings begin to disrupt your school, work, or home life, or prevent you from participating in your usual activities, it’s a good idea to speak with a trusted person. Below, we will explore some common mental health conditions that can impact how people learn, behave, and handle emotions, often making daily life a challenge.
Anxiety
We all get nervous or scared. But what if those worries never seem to go away? If constant fears start getting in the way of your life at home, school, or with friends, it might be more than just a passing feeling—it could be anxiety. Anxiety shows up in different ways for everyone, and it can look different for kids than it does for adults.
In a child, anxiety might look like:
In an adult, anxiety might look like:
See your doctor if:
Your worries may not go away on their own, and they may get worse over time if you don’t seek help. See your doctor or a mental health provider before your anxiety gets worse. It’s easier to treat if you get help early [1].
[1] Mayo Clinic. (n.d.). Anxiety. Retrieved June 27, 2025, from https://www.mayoclinic.org/diseases-conditions/anxiety/symptoms-causes/syc-20350961
Depression
Everyone feels sad sometimes. But if you’ve lost interest in activities you once loved and are experiencing persistent feelings of hopelessness or helplessness, you may be dealing with depression. Other signs of depression include:
If you are experiencing suicidal thoughts or emotional distress help is available. Call or text the national suicide and crisis lifeline at 988 or chat 988lifeline.org. There is hope.
Eating Disorders
We all have moments of concern about our appearance. But if that worry is constant and starts to impact your eating habits in a way that feels unhealthy or secretive, it’s important to know that it could be a sign of an eating disorder. Eating disorders come in many forms, and some of the signs include:
If you or a loved one are struggling with an eating disorder, call the Eating Disorders Helpline toll-free at 1 (888)-375-7767 Monday-Friday, 9am-9pm CST.
Post-Traumatic Stress Disorder
Experiencing or witnessing a traumatic event—like a car accident, a natural disaster, an act of violence, or the death of a loved one—can be incredibly difficult. While many people recover from these events, if you are still struggling after one month, you may be experiencing Post-Traumatic Stress Disorder (PTSD). Signs to look for can include:
Behavioral Disorders
Anger & Behavior:
It’s normal to disagree or argue with people sometimes—it’s a healthy part of growing up. However, if anger and irritability have become your norm, it might indicate a behavioral disorder [8]. Other signs can include frequently losing your temper and struggling to follow rules set by adults.
Attention-Deficit/Hyperactivity Disorder (ADHD):
Do you have a hard time staying focused and paying attention in class? Do you get easily distracted when working on an assignment? If so, you may be experiencing Attention-Deficit/Hyperactivity Disorder (ADHD) [9]. ADHD can make it very challenging for students to complete assignments and stay organized.
Obsessive-Compulsive Disorder (OCD):
Some young people have unwanted thoughts and urges that cause them to repeat certain actions over and over. These thoughts and actions can take up a lot of time and get in the way of daily life. This is known as Obsessive-Compulsive Disorder (OCD) [10]. An example is repeatedly checking something, like a locked door, or having to think or say the same words. If you have OCD, these thoughts and urges can be very hard to ignore, which can be frustrating.
Getting Support
If any of these conditions sound familiar, please know you are not alone. It’s more common than you might think—up to 1 in 5 children and teens experience a mental health disorder [1]. This is not your fault; these conditions can arise from complex factors that researchers are still working to understand [11]. The first and most important step to getting support is to talk to a trusted adult or friend. The sooner you reach out, the sooner you can start your journey toward mental wellness and recovery.
[8] Child Mind Institute. (n.d.). What is Oppositional Defiant Disorder?. https://childmind.org/article/what-is-odd-oppositional-defiant-disorder/ National Institute of Mental Health (NIMH). (2018, March). Autism Spectrum Disorder. https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd/index.shtml
[9] Association for Children’s Mental Health. (n.d.). Common Mental Health Diagnosis in Children and Youth. http://www.acmh-mi.org/get-information/childrens-mental-health101/common-diagnosis/
[10] Centers for Disease Control and Prevention (CDC). (2020, March 30). Obsessive Compulsive Disorders in Children. https://www.cdc.gov/childrensmentalhealth/ocd.html
[11] National Alliance on Mental Illness (NAMI). (n.d.). Teens and Young Adults. https://www.nami.org/Your-Journey/Teens-Young-Adults
Cultural DIversity
Your cultural background profoundly shapes your worldview, including how you perceive and experience mental health and its symptoms. These cultural variations extend to the effectiveness of different treatments, support systems, and coping mechanisms. Therefore, a deep awareness of these cultural differences is absolutely essential for providing appropriate and personalized mental healthcare to everyone.
It’s common to encounter cultural barriers that can make accessing mental healthcare challenging.
These can include:
Distrust or Fear of Treatment
Past experiences or cultural beliefs might lead to apprehension about seeking professional help.
Differing Views on Illness and Health
How mental health conditions are understood and perceived can vary significantly across cultures, impacting willingness to seek care.
Language and Communication Difficulties
When providers and patients don’t share a common language or understanding of communication styles, effective care can be hindered.
Limited Access
Practical obstacles like inadequate insurance coverage or a lack of affordable services can prevent people from getting the care they need.
Lack of Diverse Staff
Not seeing mental health professionals who share similar cultural backgrounds or experiences can make it difficult to build trust and feel understood.
Understanding Mental Health Disparities by Race and Ethnicity
In What Ways Does Culture Affect Mental Health?
How can you help your mental health professional understand your culture?
You can share with them:
What can the mental health professional do?
Warning Signs
Our bodies often give us important clues about our overall well-being. Think of physical symptoms like a runny nose or a cough: they’re clear red flags signaling something is amiss, perhaps the flu or another physical illness. These symptoms are your body’s way of telling you it needs help, usually prompting a visit to the doctor for medicine.
Mental health works in a similar way. Just as your body sends physical warning signs, your thoughts, feelings, or behaviors can act as red flags indicating your mental health might need attention.
While there are many such signs, here are some common ones that suggest it might be time to reach out to a trusted adult, counselor, or mental health professional:
School, family, and social lives can be incredibly rewarding, but they also present significant challenges for students. When reviewing signs that indicate a need for mental health support, some students might easily recognize several in their own lives. Certain aspects of a student’s life can make them more susceptible to these issues; these are known as risk factors.
Risk factors increase the chances of experiencing mental health problems. It’s crucial to understand that while risk factors raise the likelihood, they don’t guarantee that someone will develop a mental illness.
Risk Factors
Many factors contribute to mental health outcomes, and experiencing several risk factors can increase the likelihood of mental health challenges:
Genetics
Understanding your family’s history of mental illness is important, as a genetic predisposition can increase your own risk.
Stress
Adolescence, in particular, can bring various stressors, including peer pressure, navigating sexual identity, and the growing influence of technology.
Trauma
Experiencing traumatic events—such as physical, emotional, or sexual abuse, neglect, witnessing or being a victim of violence, or surviving natural disasters—can profoundly and negatively impact mental well-being.
Identity Issues
Adolescents exploring their gender identity or sexual orientation may face a higher risk of anxiety and depression, especially if they lack support from family or their community.
Socioeconomic Status (SES)
Socioeconomic disadvantages are recognized mental health risks. Some adolescents are more vulnerable to mental health conditions due to challenging living situations or limited access to quality support and services.
While you can’t control many risk factors like genetics or socioeconomic status (SES), you can take charge of your mental well-being by prioritizing your mental health and seeking help from trusted adults at school, such as school counselors, psychologists, or teachers.
Statistics
Annual prevalence of serious thoughts of suicide, high risk populations:
U.S. Adults: Annual Average 4.8%
Youth Populations
National Alliance on Mental Illness (NAMI). (n.d.). Mental Health By the Numbers. Retrieved July 3, 2025, from https://www.nami.org/about-mental-illness/mental-health-by-the-numbers/
Coping Skills
Coping means to face and deal with responsibilities, problems, or difficulties in a calm, appropriate and successful manner. We use coping strategies sometimes without paying attention. It is what we do to make ourselves feel better when we are upset. Coping helps us tackle our problems and find solutions like asking for help or processing strong feelings for difficult situations we cannot change.
Always remember that coping is incredibly individual – what works for one person may not work for another. This is why it’s so important to be open to trying new coping skills. Embrace the idea that your needs and approaches will change over time; the coping strategies that served you well as a child may be very different from those that support you as an adult.
While coping skills are vital for maintaining mental well-being, recognizing the need for professional support is equally important. Please refer to our resources page for assistance.
Coping Skills for Youth
Coping Skills for Adults
Building A Support System
When navigating a health condition, whether it’s physical or mental, a strong support network becomes incredibly valuable. These connections offer not just practical help, like assisting with household tasks, but also provide vital emotional support. Sharing your experiences with trusted individuals can be profoundly helpful. By cultivating a robust support system, you empower yourself to break free from unhelpful patterns, alleviate difficult emotions, and shift yourself toward healing and recovery.
What is a Support System?
A support system is a network of people or resources that an individual can rely on for various forms of help and encouragement, especially during challenging times or when striving for personal growth. It’s essentially your personal “village” that helps you navigate life. They:
A support system can be made up of a diverse group of individuals and even non-human sources:
Family members
Parents, siblings, spouses/partners, children, extended family.
Friends
Close friends, acquaintances, colleagues.
Professionals
Therapists, counselors, doctors, coaches, mentors, teachers, social workers.
Community
Neighbors, religious groups, clubs, online forums, support groups.
Pets
Many people find immense emotional comfort and support from their animal companions.
How do I build my Support System?
It may feel scary to reach out and ask for help. But everyone needs help at some point in their life. You can ask different people to help you in different ways. Start by talking with a friend or family member who:
The conversation might include:
Saint Luke’s Health System. (n.d.). Support network for mental health. Retrieved from https://www.saintlukeskc.org/health-library/support-network-mental-health
Resources
Crisis & Immediate Support
Counseling & Therapy Services
Trillium Place (Affiliated with Carle Health)
Trillium Place is a major provider of comprehensive addiction and mental health services in central Illinois, with several locations in Peoria and surrounding areas. They offer counseling, outpatient and inpatient services, and psychiatry for children, teens, and adults.
University of Illinois College of Medicine Peoria – Psychiatry and Psychology Outpatient Center
Provides diagnostic services, medication management, counseling, and therapeutic services for a wide range of mental disorders. They offer various treatment approaches, including CBT, DBT, and psychodynamic therapy.
OSF Behavioral Health (OSF Saint Francis Medical Center):
Provides support for children and adults facing acute emotional or behavioral problems.
FamilyCore
Offers counseling services to individuals and families, with specialty areas including depression, anxiety, parent-child conflicts, school problems, marital concerns, drug and alcohol issues, grief/loss, adolescence, trauma, and life adjustments.
Human Service Center
Provides a variety of mental health services, including outpatient treatment, residential treatment, and services for individuals with serious mental illness.
Gateway Foundation (Peoria)
Offers substance use disorder and co-occurring mental health treatment programs, including individual therapy and medication management for mental health concerns.
Agape Counseling
Christian counseling services.
The Antioch Group
Offers counseling and mental health services for various issues.
LifeStance Health
Offers therapy and psychiatry services for children, adolescents, adults, and new parents, treating conditions like ADHD, anxiety, depression, grief, etc. They accept most insurance plans.
Associates in Mental Health SC
A private practice with Board-Certified Psychiatrists and Licensed Therapists serving Peoria and surrounding communities.
Support Groups & Community Resources
NAMI Tri-County Illinois (National Alliance on Mental Illness)
Offers support groups for individuals with mental health conditions (NAMI Connection) and for their family members and friends (NAMI Family Support Group). They also provide educational meetings and resources.
Illinois Central College Counseling Services
Available for students experiencing mental health crisis situations during business hours.
Peoria City/County Health Department
Provides information and links to various community resources related to mental health and suicide awareness.
Children’s Home Association of Illinois
Provides emotional and mental health support services for kids between 3 and 20 years old in Peoria, Tazewell, and Woodford counties. Also offers Mobile Crisis Response.
Finding Affordable Care
OpenCounseling.com
This website lists free or low-cost counseling options in East Peoria and provides information on qualifying for state-funded counseling in Illinois.
Psychology Today
You can use their “Find a Therapist” tool and filter by “Medicaid” or other insurance types to find providers who accept lower-cost options or offer sliding scales.
Check with Providers Directly
Many clinics and individual therapists offer sliding scale fees based on income or accept various insurance plans. Always ask about costs and payment options when you first contact them.
When seeking help, it’s a good idea to call the listed numbers, visit the websites, and inquire about their specific services, accepted insurance plans, and appointment availability.

